BACKGROUND
Syringe services programs (SSPs) are integral to preventing the negative sequelae of drug use, including infectious disease and overdose.1
In 2013 there were just over 200 programs; today there are over 440.2,3
Despite their growth, programs are increasingly impacted by high demand and siloed funding. The worsening overdose crisis, and impacts of the COVID-19 pandemic, have increased demands on programs, likely increasing their costs.4
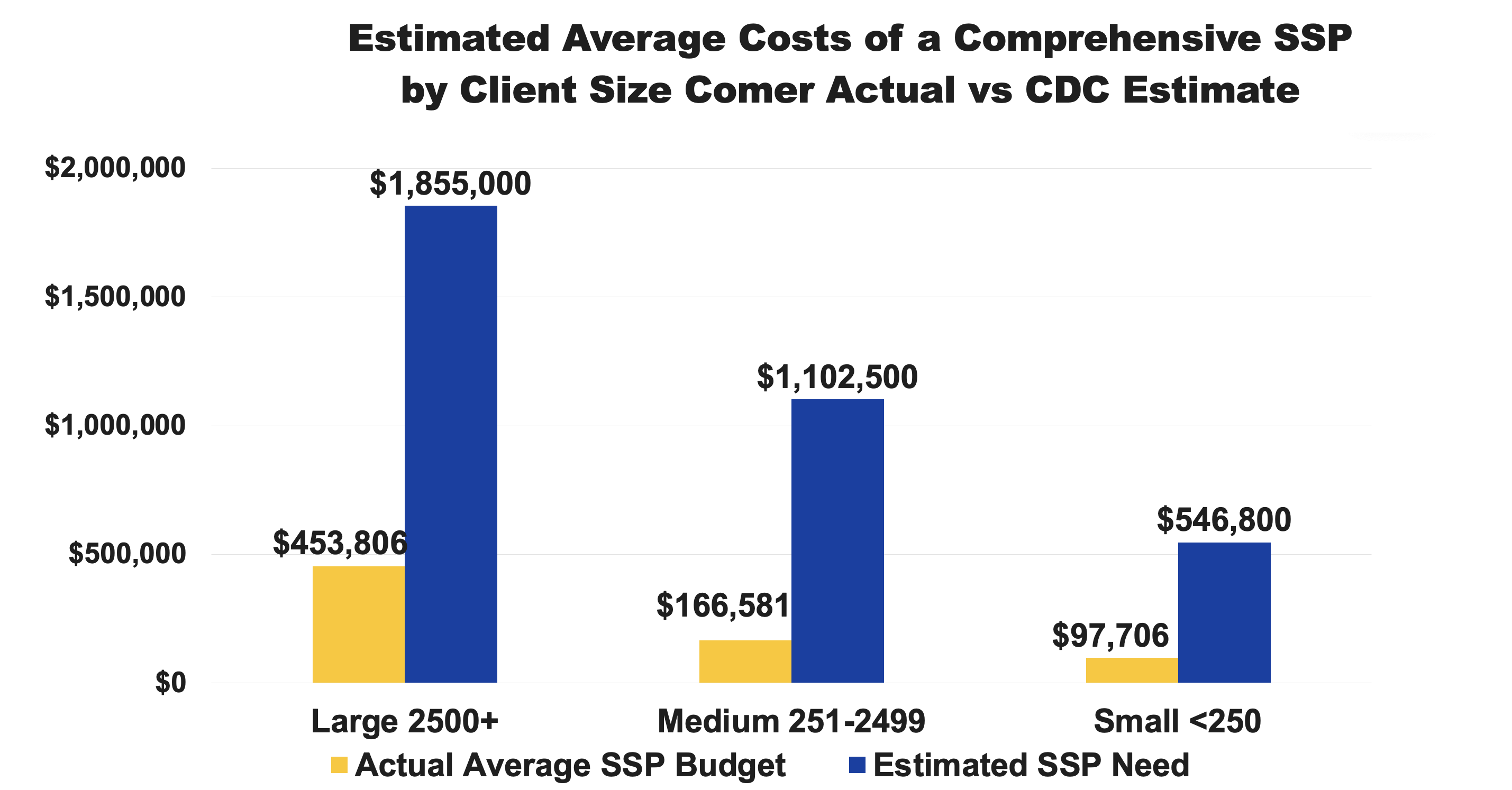
In 2019, CDC experts estimated the costs necessary to implement a comprehensive SSP serving small, medium and large populations. 5
To build on this work, Comer Family Foundation, the longest private funder of SSPs over three decades, examined the disparity between what federal experts say SSPs need to fully operate a comprehensive program against actual average program operational budgets.
This page provides a context of the current financial strains on most SSPs in the United States and what policy maker, funders and health departments should consider when funding local programs.
METHODS
We compared previously published estimated cost of a comprehensive SSP serving large, medium and small populations to 302 actual SSP budgets submitted to Comer from 2019-2022.
SSPs program size was based on the number of program participants served in the previous year
We compared the difference between average actual programmatic budgets and size and what CDC experts note estimated budgets should be to meet the needs of people who use drugs and calculated the percent difference between the two.
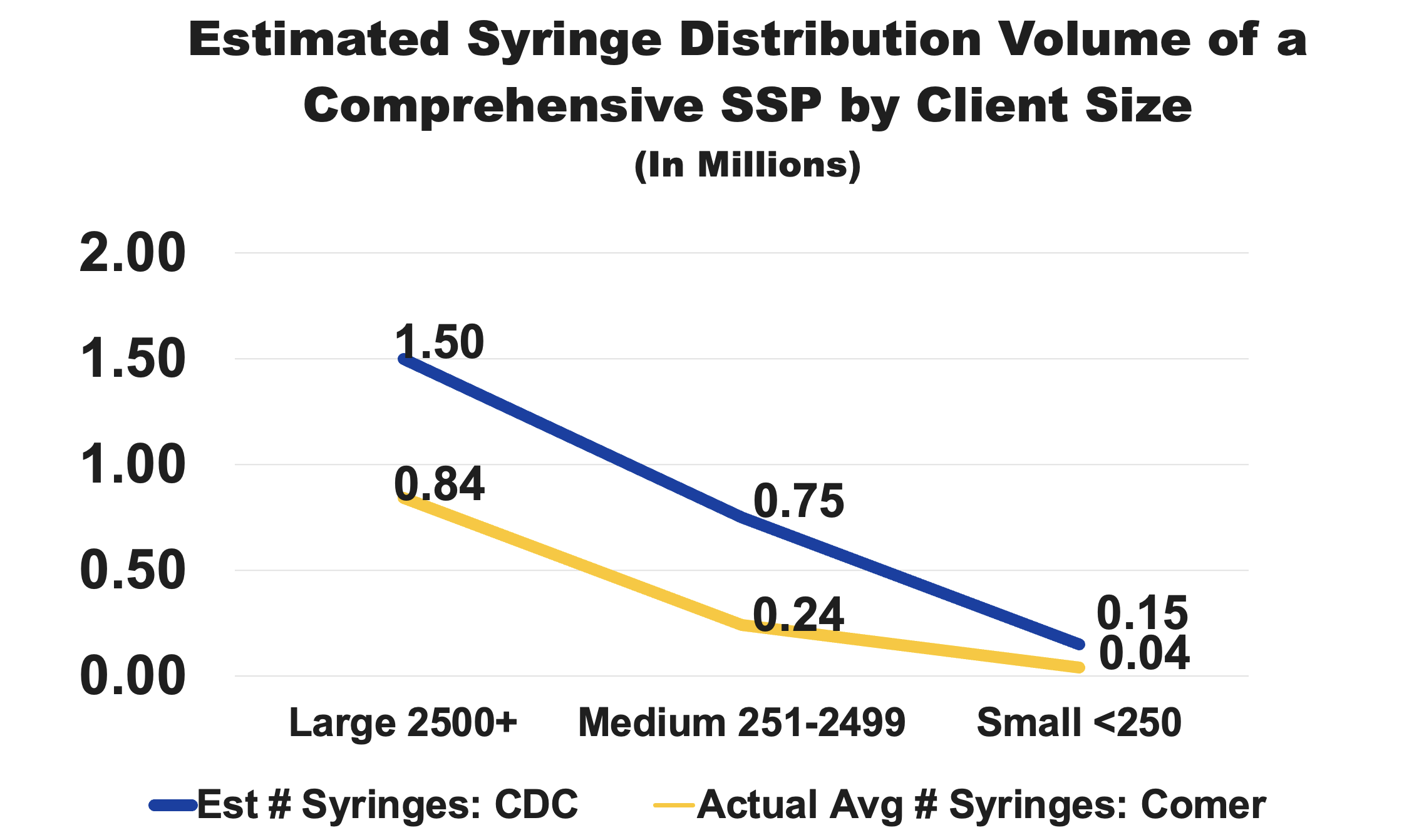
We also examined the number of syringes distributed, comparing CDC expert estimated for what is needed for full coverage and actual programmatic capacity, and top funding requests SSPs submit to the Comer Family Foundation.
RESULTS
Actual programs are operating at 24% of the budget estimated for a large SSP, 15% of a medium and 18% of a small program, suggesting they are severely and chronically underfunded.
On average, small and medium SSPs distribute less than 32% of the volume of syringes researchers estimate is needed for saturation to prevent HCV/HIV transmission.
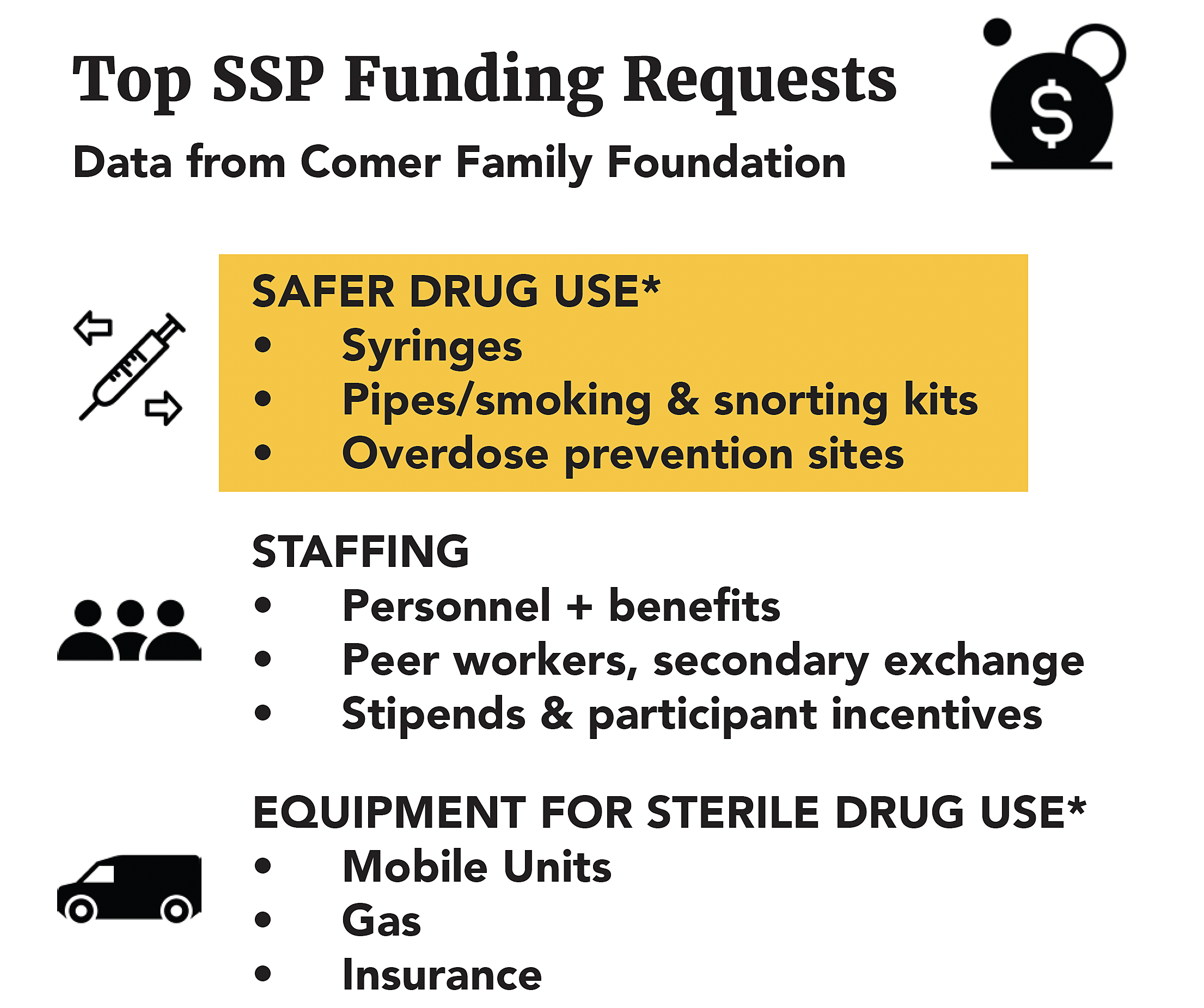
SSPs request funding for equipment, staffing and mobile services most commonly, and requests for all categories has increased since the COVID-19 pandemic.
CONCLUSION
Researcher’s analyses and Comer Family Foundation data show that smaller programs cost more per client to operate than larger sized programs. Because federal funds cannot be used to support all aspects of SSPs, these programs rely on private funders and braided funding to build comprehensive programs.
SSPs do not operate at the level of funding previously estimated they need for sustained, comprehensive work.
Despite operating on a fraction of funds needed, programs serve large number of clientele meeting their needs by funding staff at a fraction of the rate of other non-profits or relying on volunteers in order to provide equipment and services. The strain results in high staff burnout and overall risks to programs.
Policy makers, federal and private funders, health departments, and other decision makers should consider the policy restrictions and significant gaps between estimated need and actual budgets when supporting the needs of community SSPs.
REFERENCES
- Summary of Information on The Safety and Effectiveness of Syringe Services Programs (SSPs)
- Desjarlais et al, Dave Purchase Memorial 2014 National Survey of Syringe Exchange Programs: Summary of Results
- NASEN Maps
- Harm reduction and health services provided by syringe services programs in 2019 and subsequent impact of COVID-19 on services in 2020
- Estimated cost of comprehensive syringe service program in the United States